
For example, the industrial oven might lose $200 in value every month, irrespective of usage. Fixed salaries are paid consistently to full-time employees, regardless of business activity. For instance, the bakery’s manager earns $4,000 every month, whether it’s peak wedding season or a slow winter month. For example, if you pay some bills out of each paycheck, you may separate the cost out between multiple paychecks to make them easier to manage. Otherwise, you may simply make sure that you have enough cash at the start of the fixed vs variable costs month to handle them all, essentially performing a clean sweep.
- They’re the costs you can plan for and are likely already factored into your regular budget.
- SoFi does not guarantee or endorse the products, information or recommendations provided in any third party website.
- For individuals, rent on personal residences is generally not tax-deductible, with some exceptions.
- The challenge lies in balancing the need to cover this substantial fixed cost while remaining competitive in the market.
- A cost might be something like letterheads for your business, or fees that you pay to your accountant.
- It’s an all-in-one solution that enables finance managers to optimize their expense strategy, making it an invaluable tool for budget-conscious companies.
How to budget for fixed expenses
The parties may define other ways to update the rent in the contract. If you are using a screen reader, or are having difficulty reading this website, please

What is a variable expense?
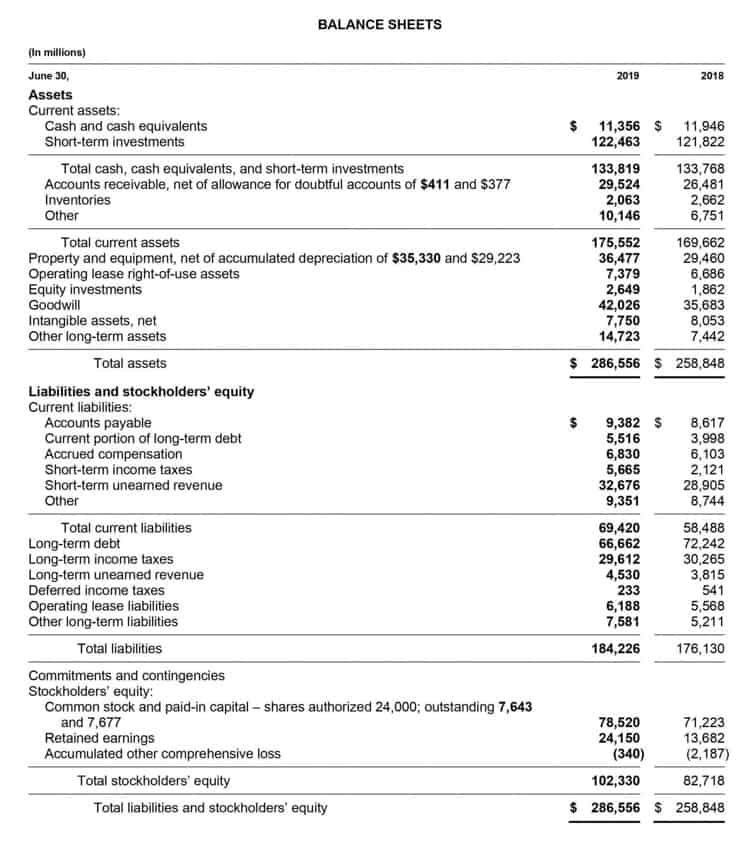
Some of these remain static regardless of output, while others will fluctuate. Understanding the differences between fixed and variable costs will allow businesses to better manage their operations, margins, and overall strategy. Marginal costs can include variable costs because they are part of the production process and expense. Variable costs change based on the level of production, which means there is also a marginal cost in the total cost of production. Fixed costs are expenses that remain the same no matter how much a company produces, such as rent, property tax, insurance, and depreciation.
Pros and Cons of Fixed Rent
Rent is generally a fixed expense, characterized by consistent periodic payments that remain unchanged regardless of business activity levels. Fixed expenses like rent are crucial for determining a business’s break-even point—the sales level required to cover all fixed and variable costs. This calculation informs pricing strategies and sales targets, especially for startups or expanding companies. Understanding fixed and variable expenses is fundamental for effective business budgeting and financial management.
- If rent on our building is $1,000 a month, and we serve 1,000 customers, then our average cost per customer is $1.
- If demand drops and production falls to zero, raw material costs also drop to zero.
- When it comes to budgeting for fixed and variable expenses, fixed expenses tend to be easier to plan for, since they are typically due at set times.
- For instance, the bakery’s manager earns $4,000 every month, whether it’s peak wedding season or a slow winter month.
- By understanding and strategically managing the impact of rent on pricing, businesses can better navigate the challenges of fixed costs and thrive in their respective markets.
- During a slow season, the store might struggle to meet its rent obligation, forcing it to cut back on inventory or staff hours, which could, in turn, affect sales—a vicious cycle.
Benefits for Tenants
A bakery spends $1.50 on raw materials (flour, sugar, etc.) for each cupcake it produces. If demand for cupcakes increases and production rises from 200 cupcakes to 400, raw material costs double from $300 to $600. If demand drops and production falls to zero, raw material costs also drop to zero. In businesses with commission-based roles, costs increase with sales. For example, if a salesperson earns a 5% commission on cupcake orders, a $1,000 order costs the bakery $50 in commissions.
- Through various case studies, we can observe the strategies companies have employed to reduce their rental expenses and how these savings have translated into overall financial growth.
- An example of this was during the 2008 Global Financial Crisis, where fixed rent leases in areas with plummeting property values became a financial burden for landlords.
- However, in cases where the rented property is unrelated to primary revenue-generating functions—such as when a company rents space for investment purposes—it may be considered a non-operating expense.
- For example, if your sales get to a point where you need to add an additional manufacturing facility your rent, property taxes and other fixed costs may rise.
- Seasonality can increase variable expenses due to higher production needs, while fixed expenses typically remain the same all year long.
You will likely pay more interest over Bookkeeping for Painters the life of the loan, but it could help you out if you are living paycheck to paycheck right now. Here, you can learn more about these two ways you spend money and how to pay less. Overall, a large part of budgeting is determining the difference between wants and needs. The best way to do this is to remember that needs are the things you can’t live without, while wants are things you enjoy but aren’t necessary to your daily life. If you have a good handle on where your money is going every month, it can help you master your budget and plan for the future. Usually, in the case of an initial reduced rent, the ISTAT adjustment starts from the year in which full ordinary rent first becomes payable.
What is a fixed expense?

Mark charges £300 per half day, and accounting his variable costs per half day, such as travelling to clients’ premises, food for while he is on site, and call charges for his mobile phone, amount to £180. Mark also has fixed costs such as his phone rental, accountancy fees and bank charges, which amount to £1,500 per month. In the realm of business finance, rent is often one of the most significant fixed costs that a company must manage.
